In cases where no obvious etiology is identifiable, a careful skin and nail-fold capillary exam is warranted. In this case, the faint scaly rash on the hands at the onset of disease was a subtle clue that prompted testing for the anti-Jo-1 antibodies. Such a rash could be easily dismissed as eczema or occupation related both by the patient and the physician. The classic rash of antisynthetase syndrome is fissured, scaly, and erythematous, located on the palmar and lateral surfaces of fingers and hand.
The patient was exposed to aerosol agents related to his occupation, though no link of the specific compounds with ILD could be made. One series of patients with antisynthetase syndrome reported 39% of subjects having occupational aerosol exposures.3 The potential role of these exposures in initiating inflammation merits further study.
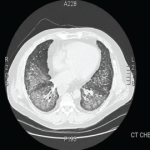
It has been suggested that antisynthetase syndrome antibodies should be tested in all patients presenting with ILD, as the presentation can be nonspecific in the early stages. This is especially true in cases with an acute presentation, NSIP pattern or lymphocytic alveolitis on histopathology, or lymphocyte predominance on BAL.3,7 Determining the antibody status may serve as a predictor of late-onset myopathy and also furnish prognostic information because anti-Jo-1 positive patients respond better to treatment, although recurrences are more common.8,9 Anti-Jo-1 seropositivity, however, does not seem to influence survival.7,8
Most treatment regimens for this condition depend on a combination of glucocorticosteroids and other immunosuppressants. Glucocorticosteroids are generally considered first-line treatment, typically at an initial dose of prednisone equivalent of 1 mg/kg, with pulmonary disease response dictating treatment duration. Other agents that have been used include mycophenolate mofetil, cyclophosphamide, cyclosporine, azathioprine, intravenous immunoglobulin, tacrolimus, and rituximab.
Dr. Aslam is a rheumatology fellow at the University of Arkansas for Medical Sciences in Little Rock, Ark. Dr. Russell is associate professor and program director at the University of Arkansas for Medical Sciences.
References
- Dalakas MC, Hohlfeld R. Polymyositis and dermatomyositis. Lancet. 2003;362:971-982.
- Kalluri M, Sahn SA, Oddis CV, et al. Clinical profile of anti-PL-12 autoantibody. Cohort study and review of the literature. Chest. 2009;135:1550-1556.
- Tillie-Leblond I, Wislez M, Valeyre D, et al. Interstitial lung disease and anti-Jo-1 antibodies: Difference between acute and gradual onset. Thorax. 2008;63:53-59.
- Mielnik P, Wiesik-Szewczyk E, Olesinska M, Chwalinska-Sadowska H, Zabek J. Clinical features and prognosis of patients with idiopathic inflammatory myopathies and anti-Jo-1 antibodies. Autoimmunity. 2006;39:243-247.
- Fischer A, Swigris JJ, du Bois RM, et al. Minor salivary gland biopsy to detect primary Sjogren syndrome in patients with interstitial lung disease. Chest. 2009;136:1072-1078.
- La Corte R, Lo Mo Naco A, Locaputo A, Dolzani F, Trotta F. In patients with antisynthetase syndrome the occurrence of anti-Ro/SSA antibodies causes a more severe interstitial lung disease. Autoimmunity. 2006;39:249-253.
- Watanabe K, Handa T, Tanizawa K, et al. Detection of antisynthetase syndrome in patients with idiopathic interstitial pneumonias. Respir Med. 2011;105:1238-1247.
- Yoshifuji H, Fujii T, Kobayashi S, et al. Anti-aminoacyl-tRNA synthetase antibodies in clinical course prediction of interstitial lung disease complicated with idiopathic inflammatory myopathies. Autoimmunity. 2006;39:233-241.
- Katzap E, Barilla-LaBarca ML, Marder G. Antisynthetase syndrome. Curr Rheumatol Rep. 2011;13:175-181.