A pathological fibrotic factor, such as CTGF, is proposed to play a role in this process. Yogarajah et al described elevated levels of CTGF in a patient with PFPAS in association with ovarian malignancy.3
Whether CTGF has any diagnostic implication is unknown at this time, as it is not a routinely ordered test. Skin biopsy from patients with PFPAS may reveal dense connective tissue, inflammatory infiltrates and immunoglobulin deposition. However, these findings are not exclusive to PFPAS. In addition, plain radiographs and magnetic resonance imaging of the hands provide limited diagnostic utility beyond what the clinical picture affords.4
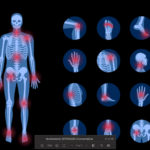
The differential diagnosis of PFPAS includes rheumatoid arthritis, scleroderma, reflex sympathetic dystrophy, Dupuytren’s contracture, diabetic cheiroarthropathy and eosinophilic fasciitis.4
Our patient lacked Raynaud’s phenomenon and had a negative ANA, which is inconsistent with scleroderma. Negative RF and CCP antibodies, coupled with DIP joint involvement, made RA unlikely. RSD is marked by symptoms of vasomotor disturbances and does not present acutely. RSD is usually seen in one extremity and is not associated with diffuse arthritis. It also typically follows an acute traumatic injury, which did not occur in this patient.
Dupuytren’s contracture is a relatively common condition and presents insidiously with nodular thickening and contraction of the palmar fascia.1 Although its manifestation can resemble PFPAS, it usually affects the ulnar side of both hands, and male predominance is common. Joint arthritis is also not a prominent feature of this condition.
Persons with longstanding and poorly controlled insulin-dependent diabetes mellitus may develop diabetic cheiroarthropathy, characterized by thickening of the digits and palmar flexion contractures producing the classic prayer sign.4 Our patient was not diabetic.
Eosinophilic fasciitis presents with myalgia and forearm thickening, which leads to palmar and finger flexion contractures.4 Peripheral eosinophilia is characteristic of this condition, but was absent in our patient.
Treatment
Anti-inflammatory drugs or corticosteroids have limited benefit in treating PFPAS-associated malignancy. Such patients do not respond to steroid treatment, but rather improve upon treating the underlying malignancy, although residual contractures may remain.3,5 PFPAS patients with no concurrent neoplasm seem to improve with steroid treatment.1

Dr. Raj
Our patient responded well to moderate doses of prednisone and was able to taper down quite steadily. Although most case reports have described the association of PFPAS with different malignancies, a few reported cases of PFPAS had no detectable neoplasm.
Seaman et al reported seven patients who developed palmar fasciitis within four months of starting the anti-tuberculosis drug ethionamide.6 The palmar fasciitis resolved when the treatment was discontinued. Another case described a 75-year-old woman who developed an idiopathic case of PFPAS. However, the possibility of a future malignancy could not be discounted because of a follow-up of just 12 months.1