At this point, we suspected TINU syndrome, given her chronic bilateral anterior uveitis and abnormal urine findings.
A percutaneous renal biopsy was peformed and revealed acute tubulointerstitial nephritis in the absence of immunoglobulin or complement deposits on immunofluorescence (see Figures 1–4). The patient was subsequently started on prednisone at a dose of 40 mg/day (1 mg/kg/day) for a presumptive diagnosis of TINU syndrome.
On one month follow-up, she reported resolution of her hand pain and swelling, and her rheumatologic exam was normal, with no evidence of synovitis. Repeat urinalysis at that point was normal. Steroid eye drops were slowly tapered down over a three-month period, and her uveitis remained quiet off of eyedrops. Repeat urine beta-2 microglobulin measurement after four months was normal at 298 µg/L (reference range: 0–300 µg/L).
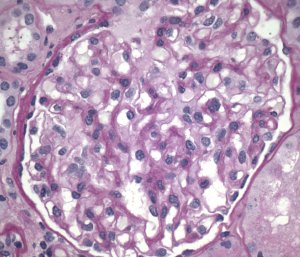
Figure 1. Normal glomeruli
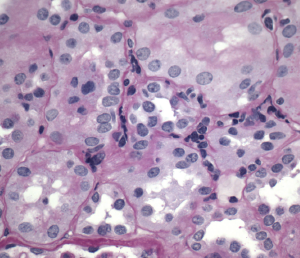
Figure 2. Interstitial inflammation
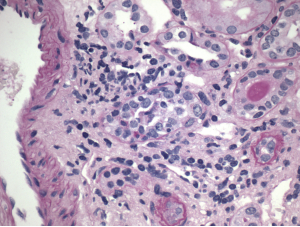
Figure 3. Tubulitis
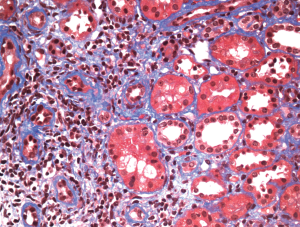
Figure 4. Minimal fibrosis
Discussion
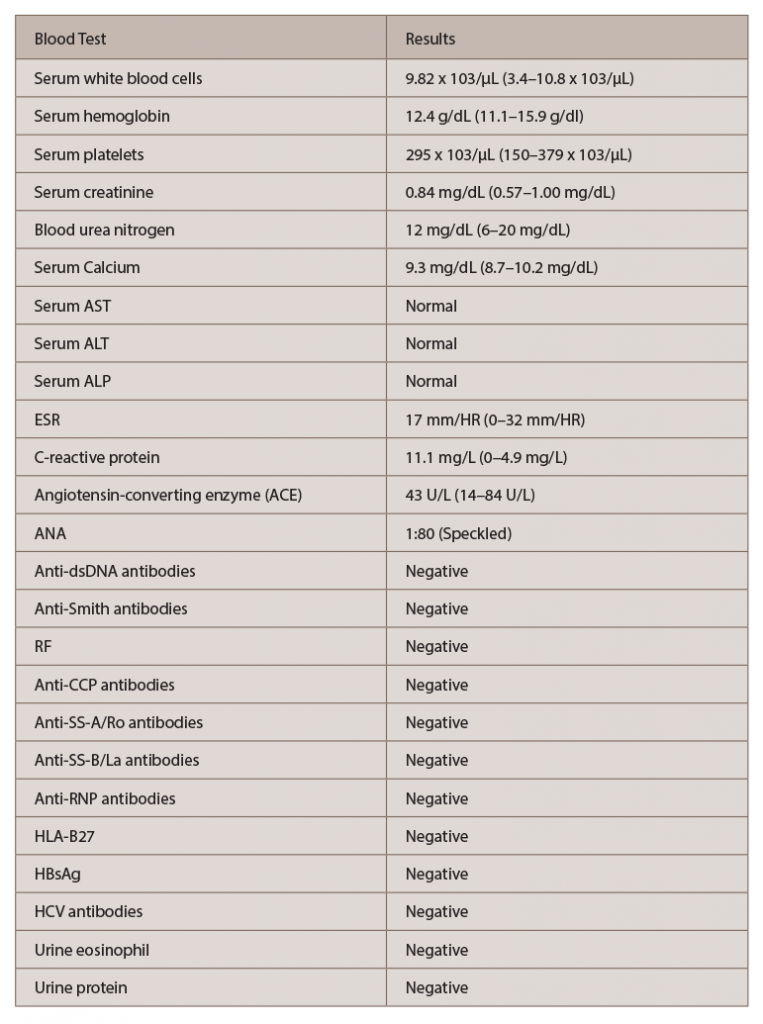
(click for larger image) Table 1: Laboratory Investigations
Key: AST: aminotransferase, aspartate; ALT: aminotransferase, alanine; ALP: alkaline phosphatase; ESR: erythrocyte sedimentation rate; ANA: antinuclear antibody; Anti-dsDNA: anti-double-stranded DNA; RF: rheumatoid factor; Anti-CCP: anti-cyclic citrullinated peptide; Anti-SS-A: anti-Sjögren’s-syndrome-related antigen A; Anti-SS-B: anti-Sjögren’s-syndrome-related antigen B; Anti-RNP: anti-ribonucleoprotein; HLA-B27: human leukocyte antigen-B27; HBsAg: hepatitis B surface antigen; HCV antibodies: anti-hepatitis C antibodies
TINU syndrome, which usually occurs in young females, is a rare condition defined by the combination of tubulointerstitial nephritis and bilateral uveitis. This disease was first described more than 40 years ago, but its underlying mechanisms remain poorly understood.
Limited evidence suggests that a common autoantigen to both the uvea and renal tubular cells (modified C-reactive protein) plays a pivotal role in its pathogenesis.5 Additionally, delayed-type hypersensitivity, with an interleukin-2 mediated proliferation and activation of T lymphocytes, has also been reported.3 Although certain risk factors, such as infection and medications, have been implicated in the onset of TINU syndrome, most often, no cause is identifiable (as in this case).4,6 Other diagnoses, such as sarcoidosis, systemic lupus erythematusos (SLE), Sjögren’s and spondyloarthropathies, should be considered and ruled out prior to diagnosing TINU syndrome.
Our patient had a positive ANA test, but negative SS-A, SS-B, anti-Smith, anti-DsDNA and anti-RNP antibodies. RF, anti-CCP and HLA-B27 were negative. Her angiotensin-converting enzyme level was normal. She also had a normal chest X-ray. Additionally, her renal biopsy was consistent with acute interstitial nephritis with no other pathological findings suggestive of SLE or sarcoidosis. After we excluded other possible diagnoses, the constellation of bilateral anterior uveitis, acute interstitial nephritis and markedly elevated urinary β2 microglobulin level confirmed the diagnosis of TINU syndrome in our patient.7,9


