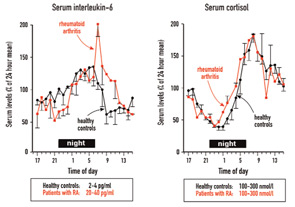
Although levels of cytokine ten times higher than normal should drive a stronger cortisol response, it is notable that the serum levels of cortisol are similar in healthy controls and patients with RA. This phenomenon is called inadequate secretion of cortisol in relation to inflammation. The reasons for this inadequacy relate in part to an inhibition of the HPA axis by chronically elevated cytokines. In other words, secreted cortisol is unable to dampen the proinflammatory response. As such, cytokine levels stay high.
What, then, is the factor that drives the nightly cytokine surge? At present, it is thought that the cortisol nadir at midnight and the parallel increase of proinflammatory hormones such as prolactin and melatonin drive the increase of nightly TNF-α and IL-6. These two cytokines drive cortisol, which finally dampens the cytokine surge, and so forth. The influence of one system on the other can be viewed as an infinite loop. Because the circadian rhythm is generated in the higher brain centers of the endocrine and nervous system (in the hypothalamus), the circadian rhythms of cytokines mirror the activity of neuroendocrine centers in the brain.
These findings are intriguing and provide a strong indication that neuroendocrine pathways influence disease-related pathophysiology. They also suggest new therapeutic options.
New Clues to Therapeutic Intervention
One would think that a therapeutic increase of circulating glucocorticoids should alleviate symptoms in patients with RA, and this has been demonstrated in Figure 1, Part A (left). These glucocorticoids are usually given after the patient awakes in the morning. One pioneering study demonstrated that administration of the same dose of prednisolone at 2 a.m. was significantly better than that dose given at 7:30 a.m. because it decreased morning stiffness, morning pain, disease activity assessed by the Lansbury index, and serum IL-6 after only five days of glucocorticoid treatment.6 These authors included two similar groups of patients with RA, who received 5.0–7.5 mg prednisolone either at 2 a.m. (therapeutic group I, n=13) or at 7:30 a.m. (therapeutic group II, n=13). Baseline values of the two therapeutic groups were very similar. No placebo group or a cross-over design was included, but the results are quite remarkable.6