The presence of a mitral vegetation on echocardiogram in our patient was a key finding that made differentiation between infective endocarditis and ANCA-associated vasculitis difficult. Cardiac involvement in GPA is rarer than involvement of other organ systems, with a prevalence reported in major studies ranging from 3.3% to 13%.11-13 However, the findings of these studies are inconsistent regarding the presence of any difference in outcomes between patients with cardiac involvement compared with those without. ANCA-associated vasculitis specifically involving the cardiac valve has been observed and appears to occur in patients with mostly C-ANCA or PR3 antibody positivity, although some cases were reported prior to the use of ANCA testing. Most commonly affected is the aortic valve, followed by the mitral valve, and pathologic assessment of these affected valves yielded nonspecific inflammation and scarring.14
Even more rare is ANCA-associated vasculitis causing vegetations on the cardiac valves, as was the case with our patient. Only a few cases have been reported in the literature (see Table 1).15-22 Our case is unique because the majority of these cases presented with aortic valve vegetations, and our patient had a mobile vegetation on her native mitral valve, which was visualized on echocardiogram.
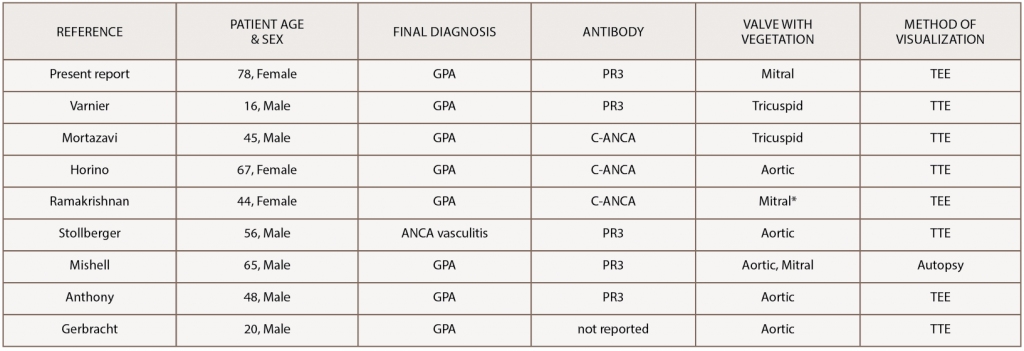
(click for larger image) Table 1: Reported Cases of GPA with a Vegetation on a Cardiac Valve
*patient had a prosthetic mitral valve from complications of previous rheumatic heart disease
GPA, granulomatosis with polyangiitis; ANCA, anti-neutrophil cytoplasmic antibody; PR3, proteinase 3; TTE, transthoracic echocardiogram; TEE, transesophageal echocardiogram
Ultimately, a combination of findings resulted in the diagnosis of GPA and initiation of immunosuppressive treatment in our patient. The renal biopsy demonstrating crescentic necrotizing glomerulonephritis without the immune complex deposits that would be expected in infective endocarditis and the finding of diffuse alveolar hemorrhage on bronchoalveolar lavage both supported GPA over infective endocarditis. The patient’s negative blood cultures and negative testing for Bartonella, Coxiella, Brucella, HIV and TB, as well as lack of response to the initial antibiotic treatment, all lowered the suspicion for infective endocarditis. The combination of these features and the patient’s response to treatment with high-dose steroids, rituximab and plasma exchange led to the final diagnosis of GPA.
Unfortunately, although the vasculitis appeared to be responding to treatment, the patient was unable to overcome her overall decompensation and, therefore, was unable to survive her illness.
Conclusions
GPA is a small vessel vasculitis that typically affects the respiratory tract and kidneys, with cardiac involvement being uncommon. Patients with small vessel vasculitis can present with signs and symptoms similar to those of infective endocarditis, and a positive ANCA can be seen in both conditions, which further complicates the assignment of a diagnosis. Vegetations on the cardiac valves are typically associated with infective endocarditis and constitute one of the major criteria for its diagnosis. However, valvular vegetations can also result from small vessel vasculitis.

