Although ophthalmologists and rheumatologists come from the same medical-school background, our training can diverge so much that even the language we speak is incompletely shared. We know many rheumatologists who stare uncertainly at the notations that are the standard nomenclature for an eye examination. And we know ophthalmologists who are unfamiliar with the new drugs—including the biologics—that are now the mainstay of immunosuppressive therapy. Given the complexity of systemic inflammatory diseases, miscommunication about ocular problems can have serious consequences, causing delays in diagnoses and even misdirected therapy.
Case for Collaboration
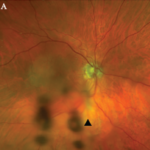
Consider, for example, the management issues raised when the the Uveitis Clinic Casey Eye Institute at Oregon Health and Science University (OHSU) in Portland recently evaluated a patient with Wegener’s granulomatosis for retinal vasculitis. The patient was a 55-year-old female with biopsy-proven Wegener’s that had been treated with prednisone and cyclophosphamide. When the patient began to develop visual loss in one eye, her Wegener’s was seemingly in remission. The dilated ophthalmologic examination, however, demonstrated widespread retinal vasculitis. This examination also revealed large patches of creamy retinal injury that are characteristic of acute retinal necrosis (ARN), a herpetic infection that is rare but much more common in an immunocompromised host (see Figure 1).
figure 1: Acute retinal necrosis from herpes virus infection.
The rheumatologic perspective was important in this case because we know that patients with a systemic vasculitis, such as polyarteritis or Wegener’s granulomatosis, rarely develop retinal vasculitis from the disease itself—especially if adequately treated. The ophthalmology perspective was equally important because the diagnosis of ARN is usually made by clinical examination that requires indirect ophthalmoscopy to identify the characteristic lesions. These lesions are often in the peripheral retina. Polymerase chain reaction (PCR) tests for a specific virus using surgically obtained ocular fluid can confirm the diagnosis. By amalgamating expertise in rheumatology and ophthalmology, we were able to appropriately diagnose this patient. The proper treatment of ARN is to reduce immunosuppression and initiate anti-viral therapy.
Ophthalmology Refresher
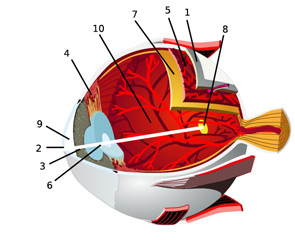
In an effort to facilitate communications with our ophthalmologic peers, this article will review the anatomy of the eye and the salient types of involvement in major rheumatologic diseases. (See Figure 2, for an overview of ocular anatomy.)