The most common symptoms of uveitis are blurred vision, pain, floaters, light sensitivity, and redness. The pain and redness are typically seen in acutely inflamed eyes, and may not be prominent in eyes with asymptomatic, chronic inflammation or for inflammation that is solely posterior to the lens. The main causes of blurred vision are media opacity from the inflammatory reaction, cataract, secondary glaucoma, and macular edema. Ophthalmologists grade and classify uveitis by severity of the inflammatory reaction and the location of ocular involvement (See table 2.)
Acute Anterior Uveitis: Spondylarthropathies
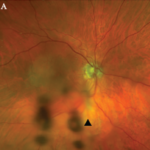
Spondylarthropathies, such as ankylosing spondylitis and reactive arthritis, are the most common identifiable causes of anterior uveitis. In North America, approximately 50% of patients with anterior uveitis are HLA-B27 positive. The typical patient presents with sudden onset of acute anterior uveitis (AAU) in one eye (see Figure 4), but this condition can subsequently recur in either eye. Simultaneous bilateral involvement is not typical. Posterior segment inflammation is generally uncommon. Most cases resolve completely within several months.3
Ankylosing spondylitis (AS): Iritis is sometimes the first clue to the presence of an associated spondylarthritis. In some patients, the inflammation can be severe enough to produce hypopyon, fibrin formation, and posterior synechiae. AAU occurs in 25% to 40% of patients with AS, and AS can be diagnosed in 18% to 34% of patients with AAU. The prognosis of AAU associated with AS is generally good; each acute attack usually responds to topical corticosteroid drops with or without cycloplegics. If promptly treated, this disease usually does not result in any residual damage to the eye.4,5
Reactive arthritis: HLA-B27–positive patients with an enthesitis also may develop episodes of AAU similar to that which occurs in patients with AS. Conjunctivitis can be seen at the early stage of the disease and acute nongranulomatous iritis occurs in approximately 40% of patients. In atypical cases, the uveitis becomes chronic, bilateral, and/or intermediate.6
Inflammatory bowel disease (IBD): Ocular inflammation occurs in approximately 4% to 6% of patients with IBD. The most common forms of ocular involvement are uveitis and scleritis. Ulcerative colitis and Crohn’s disease are both associated with uveitis. A common presentation of ocular disease resembles that which occurs in AS with nongranulomatous, recurrent, unilateral, acute anterior uveitis. Unlike AS, however, patients with IBD can have the insidious onset of a chronic, bilateral uveitis. Posterior segment involvement—including pars plana exudates, vitreous inflammation, and retinal vasculitis—has occasionally been reported.