African-American individuals with SAPHO seem to suffer higher incidences of hidradenitis suppurativa than other dermatoses.6 Dissecting cellulitis of the scalp is a rare, but reported, finding in SAPHO.4 Most commonly, SAPHO follows a self-limiting course that usually resolves within 3–12 months or, unusually, a persistent and relapsing course that frequently requires indefinite therapy.5 Rarely, it may present in a fulminant manner with simultaneous skin, joint and skeletal disease, as our patient demonstrated.
He was so stiff he resembled a statue sitting in the wheelchair.
Diagnosis is challenging because validated classification criteria and laboratory biomarkers do not exist. Two sets of classification criteria are commonly used, one proposed by Benhamou et al. in 1988, and the other proposed by Kahn and Kahn in 1994, which was then modified for presentation at the ACR/ARHP Annual Meeting in 2003.7,8
Our case fulfilled one of Benhamou’s criteria: hyperostosis of the anterior chest wall with dermatosis. It also satisfied two of Kahn’s criteria: bone joint disease associated with severe acne and sterile osteitis (Note: only one criterion is required for both proposed criteria).7,8
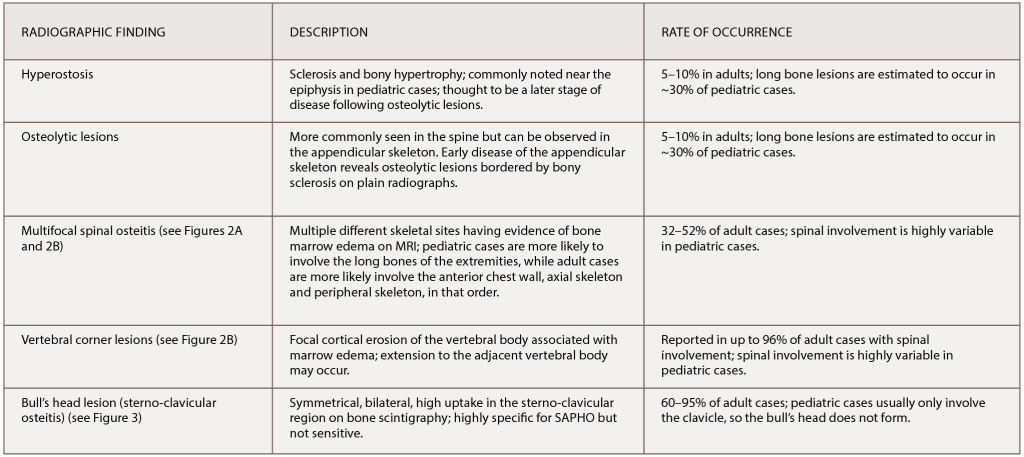
(click for larger image) Table 1: The Most Common Radiographic Observations of SAPHO Syndrome
References: Nguyen et al. (2012); Depasquale et al. (2012).
As discussed, HLA-B27 positivity did not correlate well with the diagnosis, and neither did elevations in the ESR nor CRP.3-5 Diagnosis is entirely clinical, requiring a high degree of suspicion and pattern recognition of the classic symptoms, clinical signs and imaging findings.
There is balance in the literature regarding therapeutic agents. Physicians should choose therapy on an individual basis. Several different agents have been used and suggested as efficacious by small cohorts and case reports.9 Tailoring the treatment approach to disease phenotype severity can help.
Non-steroidal anti-inflammatory drugs, oral bisphosphonates, systemic corticosteroids and conventional synthetic disease-modifying anti-rheumatic drugs all exhibit the potential to reduce symptoms and manage mild arthritis.4,9 These therapies may be used in mild cases that may spontaneously remit in the future. TNF inhibitors show especially strong potential (albeit in small trials) as remission-inducing agents, and our case highlights another successful outcome with TNF therapy for severe disease.9
Radiographic Findings in SAPHO
Classic findings on radiologic examination may be the key to early diagnosis of SAPHO syndrome due to its variability in clinical presentation. SAPHO syndrome can cause multiple different bony lesions on imaging (see Table 1), but the signature lesion is osteitis of the sterno-manubrio-clavicular articulation (i.e., the anterior chest wall syndrome). Osteitis of these four bones creates a bull’s head sign produced by the shape of hyperintensity signaling seen on bone scintigraphy (see Figure 3).

