At the three-month follow-up visit, a more detailed evaluation of her ANCA profile by Western blot analysis revealed variable reactivity to neutrophil elastase (NE) and cathepsin G (CG) in addition to PR3 (see Figure 3). At her 12-month clinic visit, the patient stated that she had completely abstained from any cocaine use and noticed no new skin eruptions. Her old skin lesions have healed with significant scarring. She is treated with HCQ 400 mg daily for her lupus symptoms consisting of intermittent arthritis flares.
Patient 2
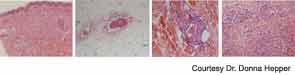
A 54-year-old white female with history of recurrent methicillin-resistant Staphylococcus aureus (MRSA) abscesses presented to the emergency department with a history of painful skin rash, fatigue, and migratory polyarthralgias involving small joints of the hands, knees, and ankles. She worked as an exotic dancer and admitted to inhalational use of marijuana and cocaine regularly. She denied intravenous drug use. Physical exam was significant for purpuric, erythematous nonblanching macules, and patches over the flexor and extensor surface of her legs, buttocks, bilateral breasts, and left pinna, including the lobe and left cheek (see Figure 4. Necrotic skin overlying these areas along with hemorrhagic bullae was noted. A workup for endocarditis was negative. The urine drug screen was positive for cocaine. Serologic testing was significant for positive ANCA 1:320 that reacted with MPO 27, PR3 11, ESR 37 mm/hr, and CRP 82 U. The infectious screen, ANA, anti-dsDNA, extractable nuclear antigen, cryoglobulins, ACL, RF, anti-CCP antibodies were all negative, and complement levels were normal. Skin biopsy findings are shown in Figure 2 and summarized in Table 1 . They revealed vasculopathic dermatitis with intravascular thrombi, dermal abscess formation over the cheek, and leukocytoclastic vasculitis with vascular complement reactivity to type IV collagen. A presumptive diagnosis of cocaine-/levamisole-associated vasculitis was made. The patient was counseled to abstain from further illicit drug use. A two-week course of oral prednisone 20 mg daily was prescribed with dramatic improvement of her skin rash, which healed with scarring.
Three months later, the patient was readmitted with a recurrence of her painful purpuric skin eruptions following the inhalation of cocaine. This time the rash was more extensive, with areas of confluence and hemorrhagic bullae. Repeat ANCA was positive at 1:1,280 with reactivity to both MPO and PR3. ANCA analysis by Western blot performed 72 hours after the event revealed strong serum reactivity against CG and PR3 with minimal reactivity toward human neutrophil elastase (NE) (see Figure 3). The patient was treated with a four-week prednisone taper resulting in complete healing of the skin lesions. Unfortunately, she continued to have relapses associated with repeated cocaine use.
Patient 3
A 41-year-old white female with a history of hypothyroidism and hepatitis C infection presented with a painful, purpuric rash with hemorrhagic bullae on her buttocks and extremities. She admitted to having smoked marijuana laced with cocaine. The urine drug screen was positive for cocaine. The ESR was 92 mm/hr, the CRP was 135 U, the ANCA was 1:640 titer with an MPO of 49 U, and the PR3 was 81 U. Serologic testing revealed a positive ANA with a titer of 1:320, in a speckled pattern. The anti-dsDNA antibody was 190 IU/ml, and the antihistone antibody was positive. The serum C3 was 115 mg/dL (normal=85–185 mg/dL) and C4 was 6.5 mg/dl (normal=12–54 mg/dL. The LAC and dRVVT were positive. Tests for HIV antibody, cryoglobulins, RF, and anti-CCP antibodies were negative. A Western blot revealed strong reactivity against CG and PR3 and moderate reactivity against human NE (see Figure 3). The skin biopsy results are shown in Table 1. She responded dramatically to a regimen of prednisone 40 mg daily for four weeks and to cessation of illicit drug use, but was lost to follow-up.
Patient 4
A 39-year-old African-American female with a medical history of MRSA hydradenitis presented with a three-day history of a painful, violaceous, bullous rash on her face, ears, extremities, chest, and abdomen. She noted five similar episodes over the past year. The urine drug screen for cocaine was positive. The absolute neutrophil count was 1.7×103/mm3, the ESR was 61 mm/hr, the CRP was 102 U, and the ANA was negative. The initial ANCA was positive with a titer of 1:1,280; the MPO/PR3 antibodies were not detectable. A repeat ANCA six months later was positive with a titer of 1:2,560 and a positive MPO of 34 U and PR3 of 47 U. The Western blot study showed strong serum reactivity against human NE and PR3 and moderate reactivity against CG (see Figure 3). A presumptive diagnosis of cocaine-/levamisole-associated vasculitis was made. The patient was counseled to abstain from further illicit drug use. Her skin lesions and neutropenia spontaneously resolved, but she relapsed six months later following repeated illicit drug use.
Discussion
Historically, cocaine use is associated with several cardiovascular morbidities due to its vasoconstrictive and platelet-activating properties. However, cocaine use also has been linked to a wide spectrum of dermatologic and rheumatologic manifestations. Table 2 (below) highlights some the common mimics of this condition, focusing on serology and histopathology. Cocaine associated midline destructive lesions may pose a diagnostic challenge and can be confused with ANCA-associated vasculitis, because the c-ANCA test is often positive in both diseases.1,2 Cocaine has been implicated in the development of acute skin necrosis, pseudovasculitis, retiform purpura, necrotizing skin lesions, Stevens-Johnson syndrome, generalized pustulosis, and cutaneous fibrosis.3,4 Recently, a vasculopathy or pseudovasculitis associated with levamisole-contaminated cocaine use is gathering increasing interest following several case reports.1,2

