 Although physicians prescribe sodium-glucose cotransporter-2 (SGLT2) inhibitors to treat type 2 diabetes, research suggests SGLT2 inhibitors may also reduce uric acid levels caused by glycosuria. This and other biologically plausible pathways have led researchers in several clinical trials to investigate whether SGLT2 inhibitors benefit adults without diabetes. Absent the results of clinical trials, some researchers have sought out real-world data to determine additional clinical applications of these drugs. Such data may be particularly useful. Since 2016, the 21st Century Cures Act directed the U.S. Food and Drug Administration (FDA) to consider the potential use of just such real-world data to help support the approval of new indications for approved drugs.
Although physicians prescribe sodium-glucose cotransporter-2 (SGLT2) inhibitors to treat type 2 diabetes, research suggests SGLT2 inhibitors may also reduce uric acid levels caused by glycosuria. This and other biologically plausible pathways have led researchers in several clinical trials to investigate whether SGLT2 inhibitors benefit adults without diabetes. Absent the results of clinical trials, some researchers have sought out real-world data to determine additional clinical applications of these drugs. Such data may be particularly useful. Since 2016, the 21st Century Cures Act directed the U.S. Food and Drug Administration (FDA) to consider the potential use of just such real-world data to help support the approval of new indications for approved drugs.
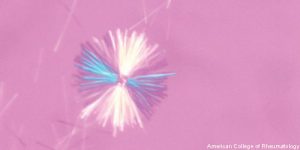
A recent study reports that adults with type 2 diabetes who are treated with an SGLT2 inhibitor have a lower rate of gout than adults treated with a glucagon-like peptide-1 (GLP-1) agonist. These findings withstood sensitivity analyses and, thus, are unlikely to be explained by unmeasured confounding factors. The research by Michael Fralick, MD, PhD, SM, a research fellow at Brigham and Women’s Hospital, Boston, and colleagues suggests SGLT2 inhibitors may reduce the risk for gout for adults with type 2 diabetes mellitus. The researchers published their findings online, Jan. 14 in the Annals of Internal Medicine.1
The longitudinal study included approximately 300,000 adults with type 2 diabetes mellitus and no history of gout. However, the investigators note that, although they excluded patients with a history of gout, the team did not have access to important gout risk factors, such as alcohol use, a purine rich diet or body mass index. Despite this limitation, the researchers used their cohort to perform a one to one propensity score matching. They were able to match patients newly prescribed an SGLT2 inhibitor to patients newly prescribed a GLP1 agonist.
Of the patients newly prescribed an SGLT2 inhibitor, 636 were subsequently diagnosed with gout (4.9 events per 1,000 person-years). Comparatively, 836 individuals who were newly prescribed a GLP agonist were subsequently diagnosed with gout (8.2 events per 1,000 person-years). Thus, the researchers found the gout incidence rate was lower among patients prescribed an SGLT2 inhibitor than among those prescribed a GLP1 agonist. They calculated a hazard ratio of 0.64 and a rate difference of -2.9 per 1,000 person-years. When the investigators performed a sensitivity analysis with as much as one year of index medication exposure, they calculated an adjusted hazard ratio of 0.73.


