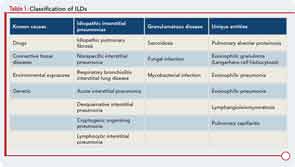
Interstitial lung disease (ILD) refers to a large group of diffuse parenchymal lung disorders characterized histologically by inflammation, fibrosis, or a combination of the two (see Table 1). Common causes of ILD include exposure to environmental antigens (e.g., avian proteins) or occupational dusts (e.g., silica or asbestos), and ILD is a common lung manifestation of connective tissue disease (CTD). Although ILD may result from any of the classifiable CTDs, patients with systemic sclerosis (SSc), poly-/dermatomyositis (PM/DM), or rheumatoid arthritis (RA) appear to carry the greatest risk for developing CTD-associated ILD (CTD-ILD). There is growing appreciation that ILD may be the first manifestation of a CTD; in fact, some experts believe that ILD may be the only manifestation of a CTD.1 In this report, we aim to discuss the epidemiology, classification, and clinical features of CTD-ILD and to highlight some areas of uncertainty and gaps in our understanding of this condition.
Prevalence of CTD-ILD
The true incidence and prevalence of ILD occurring in association with CTD are unknown. Published estimates vary because of differences in study design, in particular how cohorts are identified and the methods used to define the presence of ILD. For example, investigators who use autopsy data to confirm the presence of ILD undoubtedly overestimate the prevalence of clinically significant ILD. Prevalence estimates for CTD-ILD range from 25–90% for SSc, from 5–70% for PM/DM, from 2–63% for RA, from 8–38% for Sjögren’s disease, and from 3–38% for systemic lupus erythematosus.2 We believe that clinically significant CTD-ILD probably occurs more commonly than many rheumatologists appreciate, yet less often than pulmonologists believe. Clearly, more research is needed to better understand the epidemiology of CTD-ILD.
Classification of CTD-ILD Based on Histopathology
To characterize the histologic patterns in surgical lung biopsy (SLBx) specimens from patients with ILD, including those with CTD-ILD, pathologists use the classification scheme developed for the idiopathic interstitial pneumonias (IIPs).3 The IIPs are a group of seven ILDs of unknown cause, with potentially overlapping clinical and radiological features but different prognoses (see Table 1). Over the years, a challenging nomenclature and ever-changing classification scheme has created confusion around the IIPs. Also clouding understanding is the fact that, although the seven histologic patterns decisively distinguish one IIP from another, the patterns are not specific to “idiopathic” disease and may occur in ILD of any cause. For example, the fibrotic pattern of usual interstitial pneumonia (UIP pattern) has a number of potential causes, including chemotherapy-induced ILD, hypersensitivity pneumonitis, sarcoidosis, or any of the CTDs. The UIP pattern is the most common histological pattern in patients with IIP. However, among patients with CTD-ILD who undergo SLBx, the pattern of nonspecific interstitial pneumonia (NSIP pattern) is most frequently identified. It is unclear whether the NSIP pattern appears to predominate because of significant selection bias: relatively few patients with CTD-ILD undergo SLBx.