These findings have broadened the landscape linking infection to arthritis. Microbial pathogenesis began from the conceptual starting line that disease mediated by infection resulted from viable microbes in the target organ, as a logical application of Dr. Koch’s postulates. The discovery of the complex tango of receptor–ligand interactions involving TLRs led to the recognition that the inflammation arising as a consequence of infection requires neither a viable pathogen nor even of the intact organism. Signaling events that could usher in damaging inflammation called only for fragments of the pathogen, such as LPS or peptidoglycan, to interact with TLRs on host cells. This has been borne out in several experimental models of arthritis. The B27 transgenic rat expresses a number of features which recapitulate spondyloarthropathy (SpA) in patients, including arthritis, dermatitis, and enteritis.12 These features are dramatically attenuated if the animal is raised in a germ-free environment.13 Re-establishing the clinical features of SpA in this model does not require a gut infection in the usual sense. Rather, the animal need only be challenged with a gut commensal, Bacteroides, which would normally not be counted among the arthritogenic pathogens.
Thus, the gut being populated, not infected, with commensal organisms creates the immunological platform on which arthritis can proceed. In the postcolonial era of the twenty-first century, most find the notion of being perpetually colonized somewhat disconcerting. The interleukin (IL)-1Ra–deficient mouse is genetically programmed to develop an aggressive polyarthritis. This propensity also is completely abrogated if the animal is raised germ free.14 To re-establish the arthritis in the germ-free setting requires no intact organism at all. A TLR ligand alone will do quite nicely. These studies also have demonstrated that TLR signaling at the gut level can have very disparate effects on arthritis, with TLR4 signaling playing an exacerbating role and TLR2 signaling playing a modulatory role.
When seen in the context of concurrent genetic polymorphisms, not only in TLR but also in class I MHC and IL23-R, the infectious link between gut and joint has become intriguingly complex. This situation has become clinically relevant with the recognition that TLR2 genetic polymorphisms predispose to post-Salmonella ReA. The importance of the gut as the site of triggering events has been supported not only by the recognition that the same genetic variants confer susceptibility to AS and to Crohn’s disease (CD) but also that subclinical inflammation and upregulation of IL-23 expression is present in gut tissues of AS patients.15,16 Hematologists in search of the cause of pernicious anemia might have probed the bone marrow ad infinitum without realizing that the answer lay in the gut. Are rheumatologists destined to learn the same lesson?
Too Much—or Too Little?—of a Good Thing
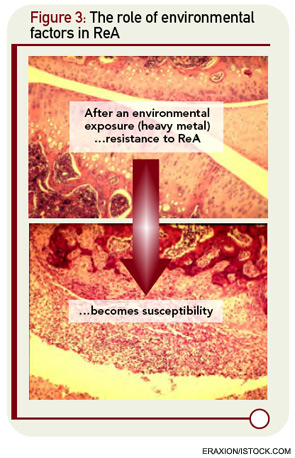
The underlying assumption in the molecular mimicry theories, exemplified by the studies of rheumatic fever, is that the host immune response to infection is overactive in nonseptic sequelae like ReA. But there are intriguing clues that host defenses might be diminished rather than amplified in patients with ReA. The cytokine profiles of ReA patients suggest down-regulation of proinflammatory cytokines rather than upregulation.17 These changes include a decrease in levels of TNF-α and IFN-γ, cytokines normally thought to be deleterious rather than beneficial cytokines with respect to arthritis. The role of cytokine dysregulation in disease etiology is borne out in experimental ReA.18 Animals that are susceptible to Chlamydia-induced arthritis have diminished rather than enhanced production of TNF-α and IFN-γ within the joint. This appears to relate to impaired capacity of host clearance of the organism in susceptible strains of animals. Of interest, this genetically defined cytokine signature can be dramatically altered by exposure to heavy metals, suggesting that other environmental factors may come into play in the dynamics of ReA in the clinical setting (see Figure 3, below right).19