NEW YORK (Reuters Health)—New European League Against Rheumatism/American College of Rheumatology (EULAR/ACR) classification criteria can be used to identify patients with systemic lupus erythematosus (SLE) in an unselected group of patients hospitalized for pericardial effusion, new findings show.1 “Overall, in patients with pericardial effusion and positive ANA, the diagnosis of SLE could be ruled out…
Search results for: antinuclear antibody
Study Finds ANA-Negative Classification Errors Among Newly Diagnosed Lupus Patients
How laboratories define a serological hallmark of systemic lupus erythematous and which assays they use to detect it could contribute to misclassification of patients identified as anti-nuclear antibody (ANA) negative, according to researchers. Most people who have lupus test positive for ANAs as part of an immunology screening for autoimmune disorders. The presence of ANAs…
Case Report: Can Salt-&-Pepper Skin Mean Systemic Sclerosis?
Systemic sclerosis (SSc) is a multi-system connective tissue disease in which skin and internal organ fibrosis are associated with an obliterative micro-vasculopathy and a degree of inflammation.1 Patients often report it takes one to three years from the appearance of the first signs and symptoms before they receive a diagnosis. The signs and symptoms of…

Did Shiitake Mushrooms Induce Immune-Mediated Necrotizing Myopathy?
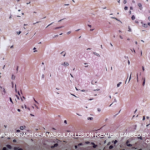
Idiopathic inflammatory myopathies are heterogenous, acquired immune-mediated muscle diseases. Over the past decade, immune-mediated necrotizing myopathy has been recognized as a subcategory of idiopathic inflammatory myopathy characterized by myofiber necrosis in the absence of prominent inflammatory cells.1 Autoantibodies against signal recognition particle (SRP) and 3-hydroxy-3-methylglutaryl-coenzyme A reductase (HMGCR) are thought to be associated with the…

Cancer-Associated Myositis: A Case Report & Review of the Literature
Since it was first reported in 1916, a correlation between inflammatory myopathies and cancer has been noted in several studies. Population studies have confirmed this relationship, and the phrase cancer-associated myopathy has entered the vernacular. Over the past decade, research efforts have shifted toward revealing associations between autoantibodies and clinical phenotypes. One subset of auto-antigens…

Uveitis: Know the Risk Factors, Symptoms & Treatment Options
Inflammatory diseases can cause uveitis. Early detection and treatment are essential, but when uveitis goes undetected it can cause blindness. Here’s how to protect your patients…

An Overview of Pediatric, Noninfectious Uveitis
Uveitis is an inflammation of the uvea, which comprises the iris, ciliary body and choroid. Uveitis can lead to ocular damage and complete visual loss. Noninfectious etiologies for uveitis are the most common in the U.S.1 The estimated incidence of uveitis ranges from 25–52 per 100,000 in adults and five per 100,000 in children. The…

New Study Works Toward Better Lupus Classification Criteria
In 1982, the ACR developed classification criteria for the identification of systemic lupus erythematosus (SLE) for use in research. The ACR updated these criteria in 1997, and in 2012, the Systemic Lupus International Collaborating Clinics (SLICC) group developed an additional set of classification criteria. In 2014, in an attempt to establish and refine even more…
Cutaneous Lupus Tied to Risk for Coexisting Autoimmune Conditions
NEW YORK (Reuters Health)—Patients with cutaneous lupus erythematosus (CLE) should be monitored closely for other autoimmune conditions, researchers suggest. Dr. Benjamin Chong, Dr. Linda Hynan and Elaine Kunzler of the University of Texas Southwestern Medical Center in Dallas analyzed data from 129 adults in the UTSW Cutaneous Lupus Registry (mean age, 49; 79% women). Individuals…

Professor Shares Findings from 45 Years of Lupus Research
SAN DIEGO—What are the predisposing genes that suggest who will develop active systemic lupus erythematosus and who will stay healthy? Decades of research data help rheumatologists clarify this picture, says Argyrios N. Theofilopoulos, MD, professor of immunology and microbiology at Scripps Research Institute in La Jolla, Calif. At his Nov. 5 lecture at the 2017…
- « Previous Page
- 1
- 2
- 3
- 4
- …
- 10
- Next Page »